Understanding BPD: Hope, Treatment, and How To Help
What you need to know about borderline personality disorder.
“Find the tools you need to heal.”
♥️A Note from Me
Hi, I’m Jessica.
I write NP Fellow, a weekly mental health and functional medicine newsletter, to help readers build emotional regulation skills, gain mental clarity, prevent burnout, and become the C.E.O. of their own health.
This article is part of a series I originally started on my Ghost blog back in 2022, where I wrote deep dives on different mental health conditions to help spread awareness and understanding.
Borderline Personality Disorder is one of the most misunderstood conditions in mental health—and one that deeply impacts emotional regulation, relationships, and sense of self. I wanted to revisit this topic with updated research, actionable coping strategies, and a hope-focused lens.
Whether you’re living with BPD, supporting someone who has it, or simply trying to understand it better, my hope is that this article helps you see that recovery is real, treatment works, and emotional regulation skills can be built over time.
Thank you for being here and for choosing to stay open to understanding.
My annual winter vibes playlist for 2026 is now out Spotify!!
🌀 NP Fellow articles will always be free.
For readers who want practical tools to build emotional regulation skills week by week, I’ve created The Weekly Skill—a structured training system for developing self-trust, nervous system stability, and psychological flexibility.
If you’d like to support this work and access The Weekly Skills, upgrade here.
Understanding BPD: Hope, Treatment, and How To Help
Borderline Personality Disorder (BPD) is one of the most misunderstood mental health conditions—and one of the most common personality disorders diagnosed today.
If you’re reading this, you might be someone living with BPD, supporting a loved one who has it, or just trying to understand what it really means. The truth is, BPD creates intense emotional experiences that can feel overwhelming, confusing, and isolating.
But here’s what matters: BPD is treatable, recovery is possible, and understanding the condition is the first step toward healing.
Today, I’m going to walk you through what BPD is, what causes it, how it’s diagnosed and treated, and how you can help someone living with it, or yourself.
Let’s dive in.
What is Borderline Personality Disorder?
BPD is marked by intense and unstable emotions, impulsive behaviors, and a pattern of unstable relationships.
People with BPD often experience a deep fear of abandonment and may see situations in extremes—what’s sometimes called “black and white thinking.”
What makes BPD particularly challenging is that it affects how someone views themselves and others.
One moment, a person might feel deeply connected to someone; the next, they might feel betrayed or rejected.
These emotional shifts aren’t intentional—they’re driven by how the brain processes emotions and relationships.
Many people with BPD are high-functioning and able to maintain jobs, relationships, and daily responsibilities.
From the outside, they may appear completely fine, but internally, they’re managing a storm of emotions that can feel exhausting and relentless.
What Causes BPD?
The exact cause of BPD is still unknown, but research points to a combination of biological, psychological, and environmental factors.
Brain structure and function: Studies show that people with BPD may have differences in areas of the brain responsible for emotion regulation and impulse control—particularly the amygdala (which processes fear and emotional responses) and the prefrontal cortex (which helps with decision-making and self-control).
Childhood trauma: Many people with BPD have a history of early trauma, including physical or sexual abuse, emotional neglect, or separation from caregivers. These experiences can disrupt emotional development and make it harder to regulate feelings later in life.
Genetic predisposition: If you have a family member with BPD or another mood disorder, your risk may be higher, but genetics alone don’t cause BPD—it’s usually a combination of factors.
Social and environmental factors: Growing up in an invalidating environment—where your emotions were dismissed, criticized, or ignored—can contribute to BPD. So can chaotic or unstable relationships during formative years.
It’s important to remember that not everyone who experiences these risk factors will develop BPD.
And people who do develop it aren’t at fault—it’s a complex condition shaped by biology and life experience.
Signs and Symptoms of BPD
BPD symptoms can vary widely from person to person, but common patterns include:
Emotional intensity: Extreme mood swings that can last hours or days—anger, sadness, anxiety, or irritability that feels disproportionate to the situation.
Fear of abandonment: A persistent fear of being left or rejected, which can lead to desperate efforts to avoid real or imagined abandonment.
Unstable relationships: Relationships that swing between idealization (”this person is perfect”) and devaluation (”this person is terrible”). This is sometimes called “splitting.”
Distorted self-image: Feeling like you don’t know who you are, what you believe, or what you want. Your sense of identity may shift depending on who you’re with.
Impulsive behaviors: Reckless actions like substance abuse, binge eating, unsafe sex, or reckless driving are often used as coping mechanisms to manage emotional pain.
Self-harm or suicidal thoughts: Cutting, burning, or other forms of self-injury. Suicidal thoughts or behaviors are common and should always be taken seriously.
Chronic emptiness: A persistent feeling of being hollow, bored, or disconnected from yourself and others.
Intense anger: Difficulty controlling anger, leading to outbursts, sarcasm, or withdrawal.
Dissociation: Feeling detached from yourself or reality, especially during periods of high stress.
If you or someone you know is experiencing these symptoms, it’s important to seek help from a licensed mental health professional.
You don’t have to wait until things feel unbearable.
How BPD is Diagnosed
BPD is diagnosed by a psychiatrist, psychiatric nurse practitioner, or licensed therapist through a comprehensive evaluation that includes a detailed patient history and symptom assessment.
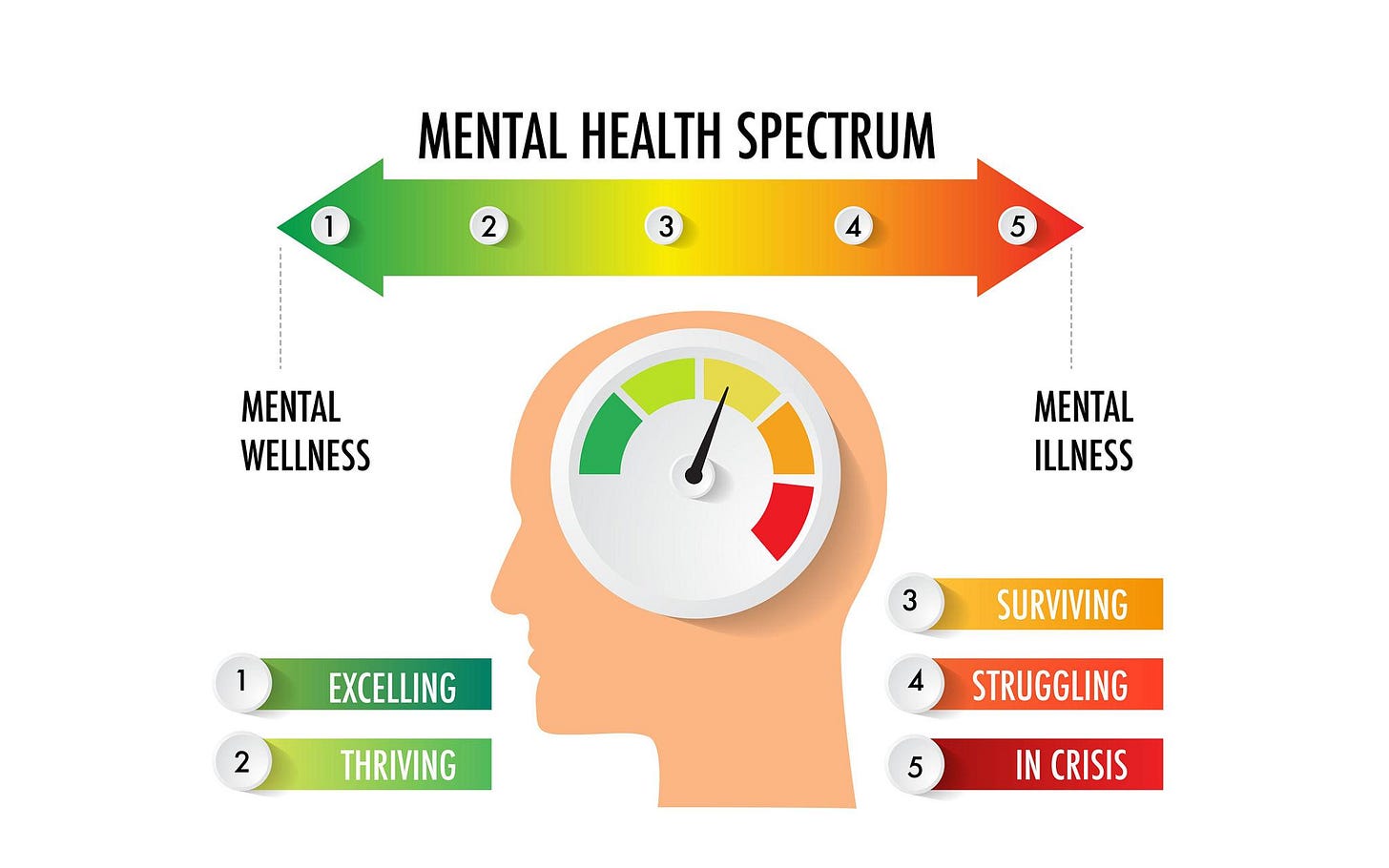
In the past, BPD was diagnosed using a categorical system—essentially checking off symptoms from a list, but mental health professionals are moving toward a dimensional approach that looks at how well someone can manage themselves in relationships and daily life.
This shift recognizes that BPD exists on a spectrum and that treatment can be tailored to individual needs.
A proper diagnosis is crucial because BPD shares symptoms with other conditions like depression, anxiety, bipolar disorder, and PTSD.
Working with a professional who understands personality disorders ensures you get the right treatment plan.
Treatment: Recovery is Possible
Here’s the most important thing to know: BPD is highly treatable, and people can and do recover.
There’s no one-size-fits-all treatment, but the most effective approaches include psychotherapy and, in some cases, medication.
Dialectical Behavior Therapy (DBT) is considered the gold standard for treating BPD. Developed specifically for this condition, DBT teaches skills in four key areas:
Mindfulness: Staying present and aware without judgment.
Distress tolerance: Managing crises without making things worse.
Emotion regulation: Understanding and controlling intense emotions.
Interpersonal effectiveness: Communicating needs and setting boundaries.
Research consistently shows that DBT reduces self-harm, suicidal behavior, and hospitalization rates. It helps people build a stable internal foundation they can rely on when emotions feel overwhelming.
Cognitive Behavioral Therapy (CBT) is another effective option. CBT focuses on identifying and changing negative thought patterns and behaviors. It’s particularly helpful for managing depression and anxiety that often accompany BPD.
Medication doesn’t treat BPD directly, but it can help manage specific symptoms like depression, anxiety, or impulsivity. Antidepressants, mood stabilizers, or anti-anxiety medications may be prescribed depending on individual needs.
Ongoing skill-building is also key. Treatment doesn’t end when therapy sessions do. Many people benefit from continuing to practice emotional regulation skills over time—whether through group support, mindfulness practices, or structured systems like the Weekly Skill, which provides a progressive framework for building emotional stability one skill at a time.
The length of treatment varies. Some people see improvement in months; others work with therapists for years.
The important thing is that progress is possible—and it compounds over time with consistent effort.
How To Help Someone With BPD
Supporting someone with BPD requires patience, compassion, and boundaries.
Here’s how you can help:
Educate yourself. Understanding what BPD is—and what it isn’t—helps you respond with empathy instead of frustration. Learn about common triggers and behaviors so you’re not caught off guard.
Validate their emotions. Even if their reaction seems extreme to you, their feelings are real to them. You don’t have to agree with their perspective, but you can acknowledge their pain. Try saying, “I can see you’re really hurting right now.”
Set clear boundaries. Compassion doesn’t mean tolerating harmful behavior. It’s okay to say, “I want to support you, but I can’t be around you when you’re yelling at me.” Boundaries protect both of you.
Encourage professional help. Gently suggest therapy or other resources. Offer to help them find a therapist or attend an appointment with them if they’re comfortable with that.
Take care of yourself. Supporting someone with BPD can be emotionally draining. You need your own support system and coping tools. Building your own emotional regulation skills—through therapy, support groups, or structured practices—helps you stay grounded so you can show up for them without burning out.
Be patient. Recovery takes time. There will be setbacks. Celebrate small wins and remember that progress isn’t linear.
Final Thoughts
BPD can feel like being trapped in your own mind—constantly fighting intense emotions, fearing abandonment, and struggling to maintain a stable sense of self.
It’s exhausting, isolating, and painful, but it doesn’t have to be a life sentence.
With the right treatment, support, and commitment to skill-building, people with BPD can build stable relationships, manage their emotions, and live fulfilling lives. Recovery is real, and it’s possible.
If you or someone you know is struggling with BPD or any other mental health condition, please reach out for help.
Talk to your primary care provider, who can refer you to a mental health professional. You don’t have to wait until things are unbearable.
And if you or someone you know is in crisis, help is available 24/7. Call or text 988 or visit 988lifeline.org to reach the Suicide & Crisis Lifeline.
Thank you for reading this article.
Until next Sunday,
—Jessica
Your 2am friend who actually gets it
“Never forget the ones who saw greatness in you even in your darkest moments.” —Yung Pueblo
🪩 A Gentle Invitation
If this article resonated with you, you may appreciate my new product called Weekly Skill, a paid NP Fellow series focused on one real, grounded internal skill each week regarding attention, distress tolerance, emotional regulation, presence, and learning how to work with your nervous system instead of against it.
No pressure. Just an invitation.🤝
🚨My new podcast NP Fellow Collective is now live on Spotify!
Recent Articles👩⚕️✍️
Looking for Quick, Mindful Workouts to Elevate Your Fitness Routine? 👇⏰💪
Check out my ebook, A Pocket Book of Express Mindful Workouts, designed to help you seamlessly integrate daily movement into your modern life.
This ebook features 20 express, mindful workouts, each just 17 minutes long, making it easy to stay active wherever you are—whether at home, in a hotel, or even outdoors.
An Express Mindful Workout combines physical movement with mindfulness, focusing on maintaining proper form and controlled breathing.
These quick routines will test your mental toughness, improve cardiovascularfitness, and build muscle strength, all while helping you develop a consistent daily workout practice.
Best of all, you can download the ebook instantly and carry it with you wherever you go.
So, no matter how busy your schedule, you’ll always have time to get moving!!
MEDICAL DISCLAIMER
This content is for informational and educational purposes only. It is not intended to provide medical advice or to take the place of such advice or treatment from a personal physician. All readers/viewers of this content are advised to consult their doctors or qualified health professionals regarding specific health questions. All viewers of this content, especially those taking prescription or over-the-counter medications, should consult their physicians before beginning any nutrition, supplement or lifestyle program.









Good read 🔥 … where can I listen to the audio version ???
I dated someone who I believe had BPD and it was HELL. I spent the entire relationship navigating a mine field. Felt like a war zone. I stayed way too long - because most people with BPD it seems don’t know or even care that they have it because everything is “everyone else’s fault.”
Great article and my hope is that those with it recognize they need help and seek out that help, and those affected by it by proximity ultimately know when to jump ship and care for their mental well-being. ❤️